Concussion Recovery: When Can Athletes Safely Return to Play?
Returning to play after a concussion isn't just about feeling better—it's about ensuring you're truly ready to get back into the game without risking further injury. As a concussion specialist, I've worked with athletes at every level—from high school to professional—helping them safely navigate the return-to-play (RTP) process. One of the most common questions I receive is: "When is it safe to return?"
The answer isn't as simple as "when symptoms are gone." It requires a strategic, stepwise approach that goes beyond symptoms, looking at brain recovery, physical readiness, and even psychological confidence. In this blog, we'll dive deep into:
What Return to Play (RTP) Really Means
The Stepwise Return to Play Protocol
Why Symptom-Free Doesn’t Mean Healed
The Importance of Baseline Testing
Exertion Protocols: The True Test of Readiness
Psychological Readiness
What Return to Play (RTP) Really Means
Return to Play, or RTP, is a structured process designed to safely transition athletes from injury back to full sport participation. The key here is "safely"—not just returning to play but doing so without an increased risk of another concussion or injury.
Returning too soon can lead to:
Repeat Concussions: Increasing the risk of prolonged symptoms and more severe injuries.
Orthopedic Injuries: Due to lingering deficits in balance, coordination, and reaction time.
Second Impact Syndrome: A rare but potentially fatal condition caused by a second concussion before the brain has fully healed.
The RTP process isn't about rushing back. It's about ensuring that an athlete can safely perform without an elevated risk of injury.
The Stepwise Return to Play Protocol
PMID: 37316210
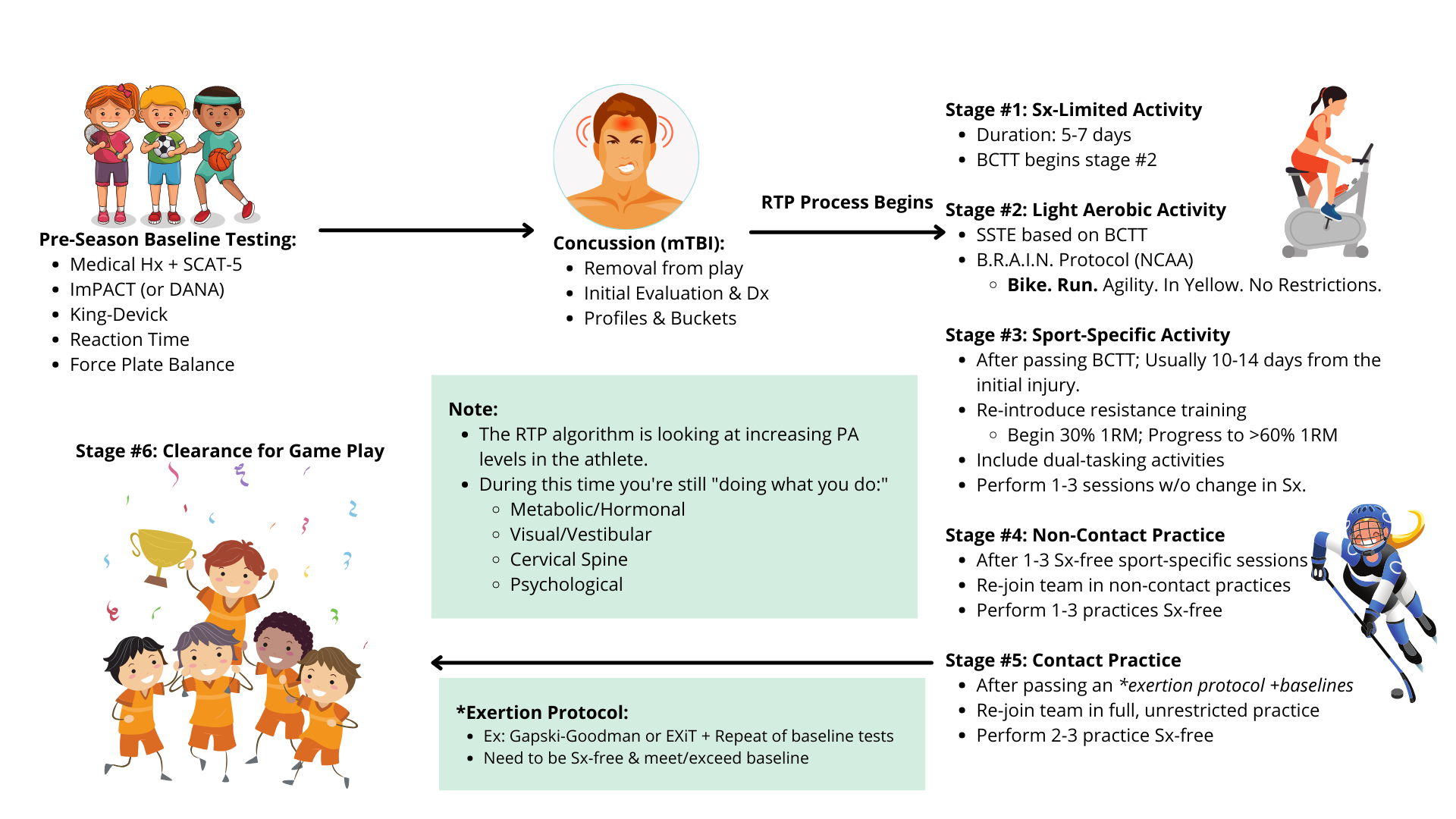
The RTP process is gradual and requires a minimum of 24 hours between each stage, ensuring no symptom flare-ups. If symptoms worsen, the athlete must step back to the previous stage and wait at least another 24 hours before progressing. Here’s the six-stage progression:
Symptom-Limited Activity:
Daily activities without triggering symptoms.
Light cognitive tasks like reading or light schoolwork.
Light Aerobic Activity:
Gentle activities like stationary cycling or brisk walking.
Aim: Increase heart rate without symptom exacerbation.
Sports-Specific Activity:
Non-contact drills related to the sport (e.g., skating drills for hockey).
Begin resistance training at 30% of 1RM, gradually progressing.
Non-Contact Training Drills:
Full practice without contact, focusing on sport-specific movements.
Dual-tasking activities are introduced to challenge cognitive and motor coordination.
Full Contact Practice:
After passing exertion protocols and baseline tests.
Engage in full contact practices to ensure game readiness.
Return to Gameplay:
Full participation in competition, confirming the athlete's ability to perform without symptoms.
Important: Any symptom worsening (more than 2 points) requires dropping back a stage and waiting at least 24 hours before progressing again.
Why Symptom-Free Doesn’t Mean Healed
Just because symptoms are gone doesn’t mean the brain has fully recovered. The neurometabolic cascade that follows a concussion involves:
Energy Deficit: A temporary drop in brain energy levels that can last 21-30 days post-injury.
Inflammation: Elevated neuroinflammatory markers that may outlast symptoms.
This means an athlete may feel fine but still have underlying deficits in:
Reaction Time
Balance and Coordination
Cognitive Processing Speed
These deficits are often linked to a 2X increased risk of orthopedic injuries (e.g., ankle sprains, ACL tears) due to impaired neuromuscular control. This is why RTP isn’t just about feeling good—it’s about being physiologically ready.
The Importance of Baseline Testing
Baseline testing isn’t for diagnosing concussions. It’s about creating a personal performance benchmark, allowing for an accurate comparison post-injury. This provides a clear picture of whether the athlete has truly returned to their pre-injury state.
Common baseline tests include:
Symptom Assessment: Using the Post-Concussion Symptom Scale (PCSS).
Cognitive Testing: ImPACT, King-Devick, or Defense Automated Neurobehavioral Assessment (DANA).
Balance Testing: Using force plates or the Balance Error Scoring System (BESS).
Reaction Time: Evaluating reflex speed and decision-making.
Why It Matters: Without baseline data, clinicians have to rely on normative values, which misclassify approximately 50% of athletes. A personalized comparison gives the highest confidence in RTP decisions.
Exertion Protocols: The True Test of Readiness
Passing baseline tests isn’t enough. An athlete also needs to pass exertion protocols to simulate the demands of gameplay. These protocols mimic the dynamic, high-intensity movements seen in sports, testing the athlete’s ability to perform without triggering symptoms.
Two highly effective protocols are:
Gapski-Goodman Protocol (Chicago Blackhawks Test):
Combines aerobic and anaerobic exertion with sport-specific vestibular and visual challenges.
Mimics real-game conditions, including rapid direction changes and dual-tasking.
Dynamic Exertion Test (EXiT):
A 30-minute clinical assessment with sport-specific movement patterns.
Evaluates physiological (heart rate, BP), performance (agility, coordination), and clinical outcomes (symptoms).
Varsity Football player working through his 2nd attempt of the Gapski-Goodman.
Why It Matters:
Research shows that even athletes who pass standard RTP stages can experience symptom flares during dynamic exertion protocols. This is why they’re crucial for a safe and confident RTP decision.
Psychological Readiness
It’s not just about physical readiness. An athlete also needs to feel mentally prepared to return to play. Even when physically cleared, a lack of confidence or fear of re-injury can:
Increase Injury Risk: Due to hesitant or overly cautious movements.
Impact Performance: As fear and anxiety affect focus and reaction time.
Work with a sports psychologist or mental health professional to assess and support psychological readiness, ensuring the athlete is both physically and mentally prepared.
Final Thoughts: When Can Athletes Safely Return?
Returning to play after a concussion requires more than just waiting for symptoms to disappear. It’s about a structured, stepwise approach that ensures:
Full physiological recovery (not just symptom resolution).
Neuromuscular control and reaction time are restored.
The athlete passes dynamic exertion protocols.
They feel confident and psychologically ready to compete.
This process is about safety, confidence, and long-term athletic health. Don’t rush it—get it right.
From my presentation at the 2022 Advanced Applications in Medical Practice (AAMP) Conference.
Need Specialist Guidance?
Navigating concussion recovery isn’t easy, especially when it comes to RTP decisions. If you’re an athlete, parent, or coach looking for a structured, evidence-based approach to concussion recovery, I’m here to help.